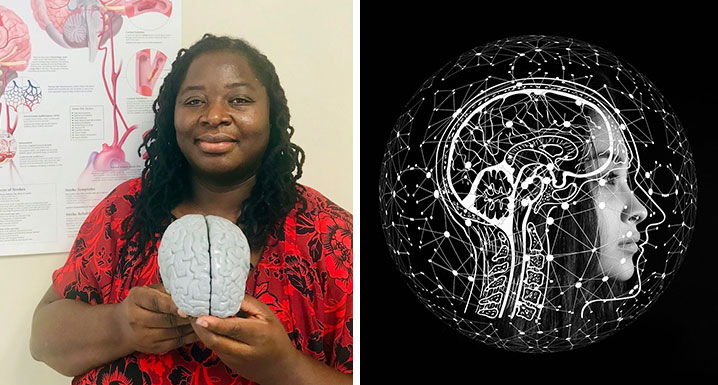
Angella Dacres is a Nurse Practitioner in the Neurology Unit, Inpatient Stroke Program at Osler. In her role, she works alongside neurologists to assess stroke patients and come up with an individualized care plan. Angella ensures patients receive the right treatment and assists with follow-up in the Stroke Prevention Clinic.
This Stroke Month, we spoke with Angella to highlight some of the most important things to know about stroke: how to identify them, who is most at risk and what to do when you experience the signs and symptoms of a stroke.
First thing’s first… what is a stroke and how does it happen?
A stroke occurs when blood stops flowing to the brain. According to Heart and Stroke Foundation, there are three main ways this can happen: a blockage or clot in a blood vessel, the breaking open of an artery, or a clot blocking an artery. This limits the flow of oxygen and glucose to the brain. The effects of the stroke depend on the type that occurs, the part of the brain that was damaged and how much damage there is.
Know the signs (and make sure your loved ones do too)
You may be familiar with the acronym FAST, used to identify the symptoms of a stroke. Knowing the symptoms, and what to do if you or a loved one experience them can result in a life saved:
- FACE: Is it drooping?
- ARMS: Can you raise both?
- SPEECH: Is it slurred or jumbled?
- TIME: to call 911
Other signs can include:
- Sudden confusion
- Sudden trouble seeing in one or both eyes
- Sudden dizziness or loss of balance, lack of coordination
Experiencing symptoms? Do NOT drive yourself to the hospital
Stroke is a medical emergency and it is not safe to operate a vehicle if you are having stroke symptoms. Please call 9-1-1. Paramedics will be able to safely transport you to the appropriate hospital for the acute stroke care needed.
Time is of the essence
When it comes to treating a stroke, acting fast is incredibly important. Every second counts; 1.9 million brain cells die every minute after a stroke occurs, so the sooner treatment is administered and blood flow returns, the greater the chance of a positive recovery.
There is a four and a half hour window where a specific treatment (Thrombolytic drug such as TPA - tissue plasminogen activator) can be given to stop the blood clot which is causing the stroke. If this is administered in time, it can save lives and improve the after-effects and impact of the stroke. Don’t wait. If you are experiencing symptoms, go to the hospital immediately.
Who is most at risk of stroke and what can they do to prevent it?
Those who have high blood pressure, diabetes and high cholesterol are most at risk for stroke. To minimize the risk, maintaining a healthy lifestyle is key.
- Eat sufficient vegetables and fruits, low fat dairy products and reduce your salt intake
- Exercise regularly – aerobic activities like walking, jogging, cycling, 3-5 times a week for at least 30-60 minutes is key
- If you smoke, take measures to quit and decrease alcohol consumption
When taking stroke medication, consistency is key
Stroke medications are used to either prevent or treat a stroke. Either way, consistency is extremely important when taking stroke medication.
Some tips:
- Take medications as prescribed. Do not stop taking them without speaking to your doctor or pharmacist.
- Know the name and dosage of medications you are taking. Keep a list with you at all times.
- Set a routine and follow it closely. Ask your pharmacist for a blister packs to make it easier to remember when to take the medications.
- Avoid mixing prescribed medications. If you must, speak with your doctor or pharmacist first to ensure there are no negative interactions between medications.
- Report any side effects experienced while taking medications
Other medication used to treat the risk factors of high blood pressure, diabetes, cholesterol associated with stroke should not be discontinued without the advice of a medical practitioner.

